Streamline your credentialing process with our comprehensive provider enrolment services. We handle the complexities so you can focus on delivering exceptional patient care.
What is Medical Credentialing?
Understanding the foundation of provider enrollment
Medical credentialing is the process of verifying and assessing the qualifications of healthcare providers. It involves thorough verification of education, training, licensure, certifications, and work history to ensure providers meet industry standards and payer requirements.
Provider enrollment is the subsequent step where credentialed providers are enrolled with insurance payers, allowing them to bill for services and receive reimbursement. This critical process can take 90-180 days and requires meticulous attention to detail and ongoing maintenance.
Why Choose Our Credentialing Services?
Expert guidance through every step of the process
Save Time
Focus on patient care while we handle the complex credentialing process.
Reduce Errors
Our expert team ensures accurate and complete applications every time
Faster Approval
Expedited processing with established relationships with major payers.
Compliance Assured
Stay current with ever-changing credentialing requirements and regulations.
Comprehensive Credentialing Solutions
Full-service credentialing and enrollment support
Provider Enrolment
Complete enrolment with Medicare, Medicaid, and commercial insurance payers.
Hospital Privileges
Assistance with obtaining and maintaining hospital staff privileges and credentials
CAQH Management
Set up and ongoing maintenance of your CAQH ProView profile with timely attestations.
Re-Credentialing
Proactive management of re-credentialing timelines to prevent coverage lapses.
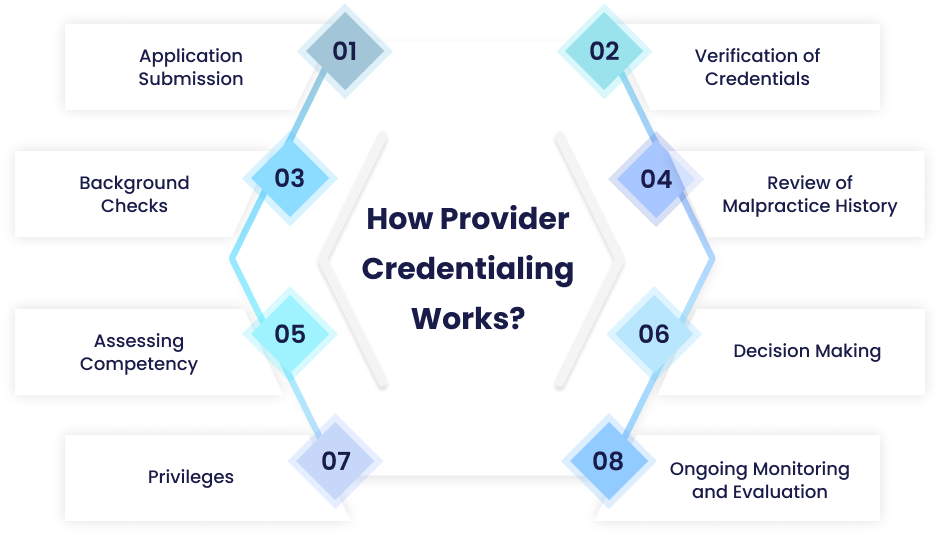
Our Credentialing Process
A systematic approach to seamless provider enrolment.
Initial Assessment
We gather all necessary provider information, licenses, certifications, and documentation required for credentialing.
Application Preparation
Our team prepares and reviews all credentialing applications, ensuring accuracy and completeness before submission.
Payer Submission
We submit applications to insurance payers, hospitals, and other healthcare organizations on your behalf.
Follow-Up & Tracking
We monitor application status, respond to requests for additional information, and keep you updated throughout the process.
Approval & Maintenance
Once approved, we maintain your credentials, track expiration dates, and handle re-credentialing to ensure continuous coverage.
Specialties We Serve
Credentialing expertise across all medical specialties
Ready to Streamline Your Credentialing?
Let our expert team handle your credentialing and provider enrollment so you can focus on what matters most—your patients.